Colorectal Cancer in GCC Gulf Countries – Diagnosis and Management: Expert Recommendations

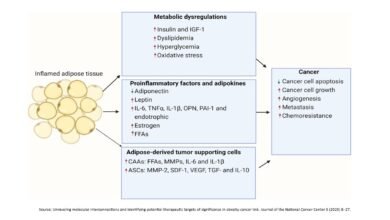
Colorectal Cancer in GCC (Gulf Cooperation Council) countries has incidence rates from 9.9 to 15.9 per 100,000 people. Experts are concerned about a rising trend, especially in individuals less than 50 years old, linked to rapid urbanization, poor diet, low physical activity, and increased hereditary risk due to a high rate of consanguineous marriages.
Survival rates in the Gulf are lower than in North America and Europe, mainly due to suboptimal screening uptake due to limited public awareness & cultural barriers, delay in diagnosis due to locally unavailable molecular testing facilities, economic hurdles faced by expatriates with low-income, and inconsistent adherence to international guidelines.
To reduce the disparity in CRC outcomes between the Gulf region and Western countries and to address current evidence gaps in practice, expert opinions were gathered from key opinion leaders in the region.This article summarizes these expert opinions to help clinicians make informed decisions, and guide the management of CRC in the GCC region.
Recommendations for CRC Screening
- All patients aged ≥45 years should be screened. Patients with a family history of CRC or Lynch syndrome should begin screening at 25 years.
- Regular screening for patients with Inflammatory Bowel Disease, Crohn’s disease, ulcerative colitis) and obesity/overweight.
- Colonoscopy as gold-standard for screening. FIT is also recommended in some countries based on patient conditions.
- National screening campaigns with general population participation and through social media campaigns.
- Collaboration between primary care physicians and specialists to implement screening and early diagnosis.
Recommendations for Molecular Testing
- Molecular testing for all metastatic CRC (mCRC) patients upon diagnosis.
- Recommended mutations to be tested for mCRC include KRAS, HER2, BRAF, and MSI/MMR. In some cases, KRAS G12C is advisable.
- For all early CRC cases, testing of MSI/MMR should be performed.
- Setting up molecular testing facilities within each GCC country
- Molecular testing is recommended in cases of early-stage CRC progressing to the metastatic stage. In some cases, molecular testing is advised for refractory mCRC
Recommendations for Treatment Guidelines
- Treatment should be based on tumor characteristics, tumor sidedness, molecular profile, patients’ performance status, comorbidities, and preferences.
- Adjuvant Therapy advised for Stage 3 and high-risk Stage 2 disease and should be continued for 3–6 months based on risk stratification.
- First-Line Chemotherapy with doublet (FOLFOX or FOLFIRI) or triplet (FOLFOXIRI) therapy is recommended based on patient and tumor factors.
- In the case of KRAS wt and BRAF wt patients, anti-EGFR + chemotherapy is advised for left-sided tumor and anti-VEGF + chemotherapy for right-sided tumors.
- Targeted therapy for patients with BRAF and HER-2 mutations is recommended in the second- and third-line settings. For patients with no actionable mutations, regorafenib or tipiracil/trifluride is recommended in the third line (regorafenib, or regorafenib + nivolumab, lonsurf/ bevacizumab).
For patients with high MSI and deficient MMR, immune therapy is recommended for locally unresectable CRC as neoadjuvant treatment and for metastatic CRC as a palliative first-line of treatment. - Treatment of mCRC patients with liver metastasis should be individualized and managed by a multidisciplinary team.
- Re-challenging anti-EGFR monotherapy in positive ctDNA assays after initial treatment with an EGFR agent and in CRC progressing after the last anti-EGFR-free regimen.
Follow-Up
- Early CRC patients should be followed for up to five years. Scans and colonoscopy are advised for the first 2–3 years. Lab investigations (CBC, liver profile, tumor markers) should be performed at every visit.
- Patients with stages 2–3 CRC receiving adjuvant therapy should be referred to surveillance clinics every three months for the first two years, every four months in the third year, and every six months from the fourth year onward
Roadmap for Future Management
Future efforts must address logistical challenges, including the shortage of specialized professionals and uneven access to advanced facilities. Key priorities are:
- Research: Understanding the unique genetic/molecular profiles and optimizing non-invasive, cost-effective screening methods (stool DNA, blood biomarkers).
- Treatment & Prevention: Investigating new CRC vaccines and promoting lifestyle modifications (diet, physical activity) to reduce recurrence.
- Collaboration: Establishing a Gulf Cancer Research Consortium for regional collaboration, data sharing, and developing uniform guidelines to standardize protocols across the region.
Reference Source:
Humaid O Al-Shamsi, Kakil Rasul Snr, Alaaeldin Shablak, Abdulsalam ALnajjar, Amrou Mamdouh abdeen Shabaan, Maha Al Sindi, Michael Nasr, Ali AlJabban & Saeed Rafii (2025) Diagnosis and Management of Colorectal Cancer in the Gulf Area: Current Practice and Future Suggestions from Expert Opinions, OncoTargets and Therapy, 1265-1279, https://doi.org/10.2147/OTT.S535858