Lipoprotein(a) Knowledge, Awareness, and Clinical Practice Among Physicians in the Arabian Gulf Region

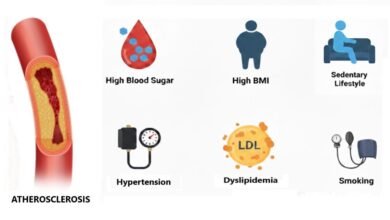
A study of 1069 physicians across the Arabian Gulf region (Saudi Arabia, Oman, United Arab Emirates, Qatar, Kuwait, and Bahrain) revealed a general limited knowledge and awareness of Lipoprotein(a) (Lp[a]). Lp(a) is a promising biomarker with the potential to improve atherosclerotic cardiovascular disease risk assessment.
The overall mean knowledge score was modest (M = 9.0 ±3.5) out of a possible score of 17.0. Furthermore, a significant majority of participants a (75%) either self-reported as being unaware of or “neutral” regarding their awareness of Lipoprotein(a). This knowledge gap could potentially lead to the underestimation of cardiovascular risk in patients
According to the US Centers for Disease Control and Prevention, Lp(a) levels > 50 mg/dL (125 nmol/L) are regarded as high and should warrant further investigation and management. Only 37% of participants correctly identified the high-risk cutoff levels.
Almost a quarter of the participants were not aware of myocardial infarction and stroke as complications of elevated Lp(a), and almost half were not aware of heart failure and aortic stenosis as complications. A significant proportion of our participants chose incorrect complications of Lp(a), such as cancers (23.2%) and inflammatory bowel disease (18.3%).
Almost half (47.9%) of physicians surveyed worked in tertiary care settings. Internal medicine was the most represented specialty (25.8%), followed by family medicine (19.7%) and cardiology (17.8%). Knowledge scores varied significantly across different demographic and professional groups:
- Cardiologists had the highest mean knowledge score (M=10.91) followed by endocrinologists.
- Tertiary care practitioners had marginally better knowledge scores than primary care physicians (9.38 vs 8.78).
- Physicians over age 45 years had the highest knowledge levels and clinicians with more than 15 years of experience scored higher than those with five years or less experience.
Despite these differences, the study noted a discrepancy where, regardless of the claimed awareness level, participants generally remained within the modest knowledge category, suggesting that self-assessed awareness doesn’t accurately predict basic knowledge of Lp(a) targets or its role in ASCVD.
A substantial proportion of physicians (76.4%) reported they had never ordered Lp(a) level measurements. The main reasons cited for not ordering were lack of sufficient information (31.2%) and unavailability in hospitals (23.9%).
Statins were viewed by 55.6% of participants as the best initial approach to lowering Lp(a). This is concerning, as statins have been reported to increase (Lp[a]) levels by 10% to 15%. The Lp(a) lowering medication pelacarsen was not commonly selected as first-line.
The authors recommend an urgent call to action for healthcare policymakers to increase awareness about Lp(a) through educational campaigns, webinars, and conferences. They also recommend making Lp(a) testing available and affordable to yield increases in screening for this risk factor.
Reference Source
Alhabib et al., Lipoprotein(a) knowledge, awareness, and clinical practice among physicians in the Arabian Gulf region, Journal of Clinical Lipidology, https://doi.org/10.1016/j.jacl.2025.09.034