Association of SMuRFS with Cardiovascular Risk Factors, Disease Burden and Pharmacological Management in Middle Eastern Patients
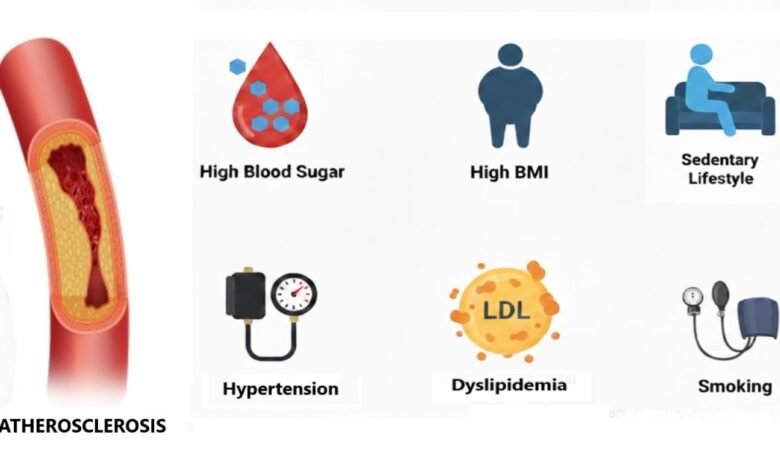
A study published by researchers from Jordan, Saudi Arabia, and Qatar has shed light on how Standard Modifiable Risk Factors (SMuRFs) such as smoking, hypertension, diabetes, and dyslipidemia cluster to accelerate disease progression and increasing the risk of severe outcomes like myocardial infarction and heart failure in Middle Eastern patients.
The study comprised of 1,859 patients with a family history of ASCVD and premature cardiovascular issues. Researchers integrated data from six regional cardiovascular registries and the Jordan SMURF-less cohort into a single harmonized database.
Patients were divided into three groups based on their risk factor count:
- Group 1 (SMuRF-less / 0 SMuRF): No risk factors.
- Group 2 (1–2 SMuRFs): Moderate risk clustering.
- Group 3 (3–4 SMuRFs): High risk clustering.
Clinical Characteristics and Risk Factor Clustering
The findings revealed significant demographic and clinical differences between the groups:
- Higher SMuRF burden correlates with age. The high-risk group had a mean age of 57.1 years, whereas the SMuRF-less group averaged 51.9 years.
- Comorbidities increase in step with SMURF counts “clustering effect”. Chronic kidney disease (CKD) and heart failure were notably more prevalent in Group 3.
- Body Mass Index (BMI) showed a direct upward trend with SMuRF counts. The highest-risk group reached a mean BMI of 29.3 kg/m², placing them in the obese category.
- Higher SMuRF counts were also directly associated with Elevated Triglycerides and Higher LDL Cholesterol. These findings suggest that for regional patients, managing triglycerides may be just as vital as managing LDL levels to prevent major adverse cardiac events.
Pharmacological Management and Treatment Trends
The study observed that medication use was highest among patients with the greatest number of modifiable risk factors. Statins and aspirin were widely prescribed, with usage rates reaching 94.8% in Group 3 compared to 87.5% in the SMURF-less group. Beta-blocker usage followed a similar trend, prescribed to 76.0% of patients in Group 3 to manage hypertension and prevent arrhythmias.
Oral hypoglycemic agents were prescribed for 28.6% in Group 3. The significantly increased use of oral hypoglycemic medication in multiple cases in the SMuRF represents an increased need for strict glycemic and cardiovascular risk control in the population in the Middle East, where diabetes has been reported to be as high as 22 -33% in some countries. In response to this challenge, sodium-glucose cotransporter 2 (SGLT2) inhibitors and glucagon-like peptide-1 (GLP-1) receptor agonists are recommended for managing cardiovascular risk in patients with diabetic ASCVD
Conclusion and Regional Implications
The study confirms that SMuRFs cluster and exacerbate vascular damage, accelerating the progression of ASCVD. It reinforces the critical need for early, targeted, and culturally tailored cardiovascular risk reduction strategies in the Middle East, particularly among individuals with a family history of premature CVD.
Article summarized and edited by Dr. Parvin Aktar Barbhuiya
Reference Source: Alrida, N. A., Albikawi, Z., Alotaibi, N., Alkouri, O., Saifan, A. R., Jarrah, M., Hammoudeh, A., Khader, Y., Alenezy, A., Al-Zu’bi, B. M., Alharbi, A., Alhalaiqa, F., & AbuRuz, M. E. (2025). Association of SMURFs with cardiovascular risk factors, disease burden, and pharmacological management in Middle Eastern patients with ASCVD and a family history of premature CVD. Frontiers in Cardiovascular Medicine, 12, 1678767. https://doi.org/10.3389/fcvm.2025.1678767